Back pain is one of the most common reasons people visit a doctor or miss work, and it’s also a leading cause of disability worldwide. When the pain becomes severe or persistent, it’s natural to want answers and fast. For many that means turning to imaging tests like X-rays, MRIs, or CT scans in hopes of finding the root cause. But here’s the surprising truth: most of the time, scans don’t actually explain back pain.
Let’s explore why.
1. Lower Back Pain Often Has Non-Structural Causes
Lower back pain isn’t always caused by something that can be “seen” on a scan. Many cases of back pain are related to:
- Muscle strain
- Ligament sprains
- Poor posture
- Stress and tension
- Lack of movement or deconditioning
Lower Back Pain – MRI shows nothing
These are real painful problems but they don’t usually show up on imaging. A scan might look completely “normal” even if you’re in significant pain.

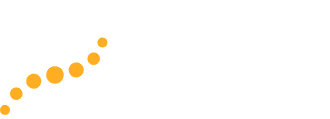
2. Many Abnormalities Are Found in Pain-Free People
This is one of the most important and misunderstood points: scans often show things that aren’t causing pain. Multiple studies have shown that people with no back pain at all often have:
- Bulging or herniated discs
- Degenerative disc disease
- Spinal stenosis
- Arthritis
For example, research has found that up to 50% of people over age 40 with no symptoms had disc bulges on MRI. These findings increase with age and are often just part of the natural aging process not necessarily the source of pain.
So, just because a scan shows a disc bulge doesn’t mean it’s what’s hurting you.
3. Scans Can Lead to Misdiagnosis and Unnecessary Treatment
Once something is found on a scan, it’s easy to focus on it even if it’s not causing the problem. This can lead to:
- Anxiety about the “damage” seen on the scan
- Over-reliance on passive treatments
- Unnecessary surgery
- Use of opioids or invasive procedures
In many cases, people get better with time, movement and self-care regardless of what a scan shows.
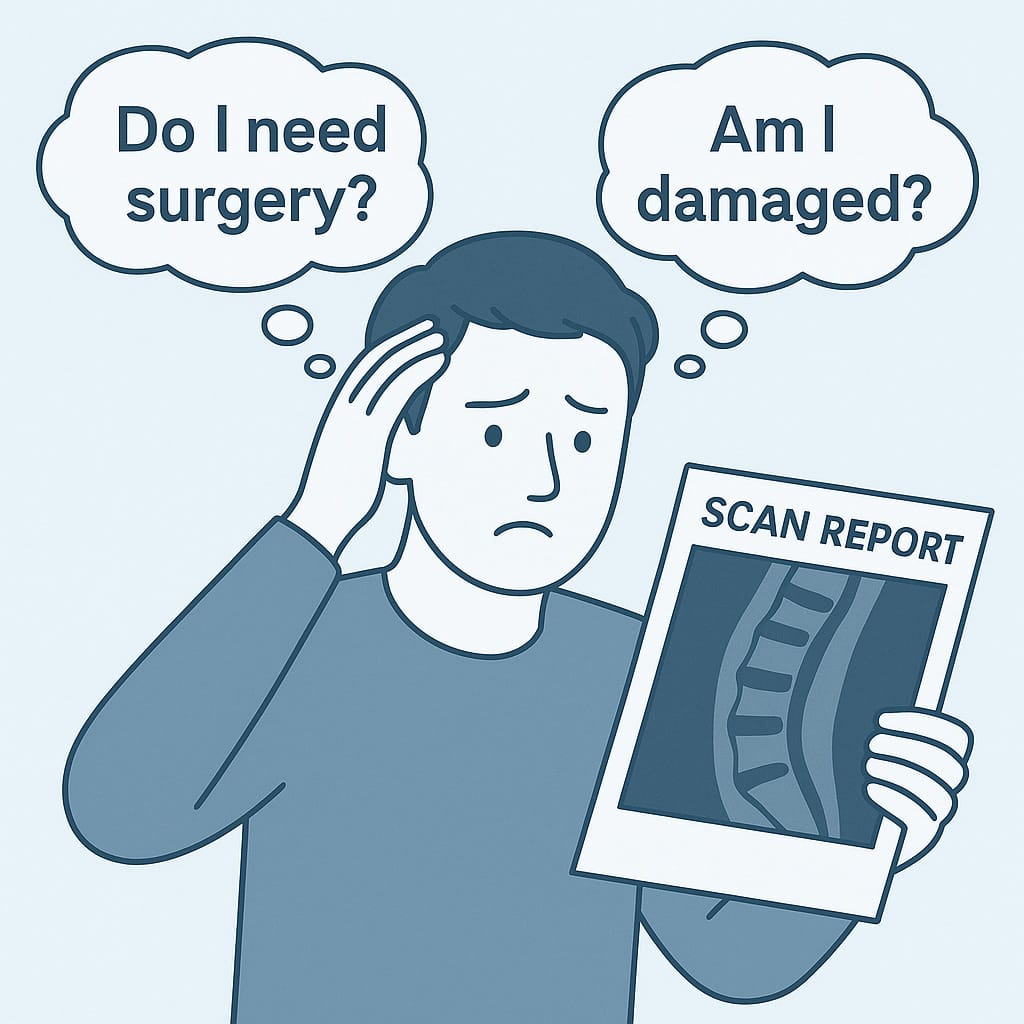
4. Pain Is Complex and Involves the Nervous System
Pain isn’t just about structural damage; it also involves how your brain and nervous system interpret signals from the body. Factors like stress, fear, lack of sleep, or past trauma can amplify pain signals even if there’s no serious tissue damage. This doesn’t mean the pain is “in your head,” but it does mean that imaging alone can’t tell the full story.
5. When Are Scans Actually Helpful?
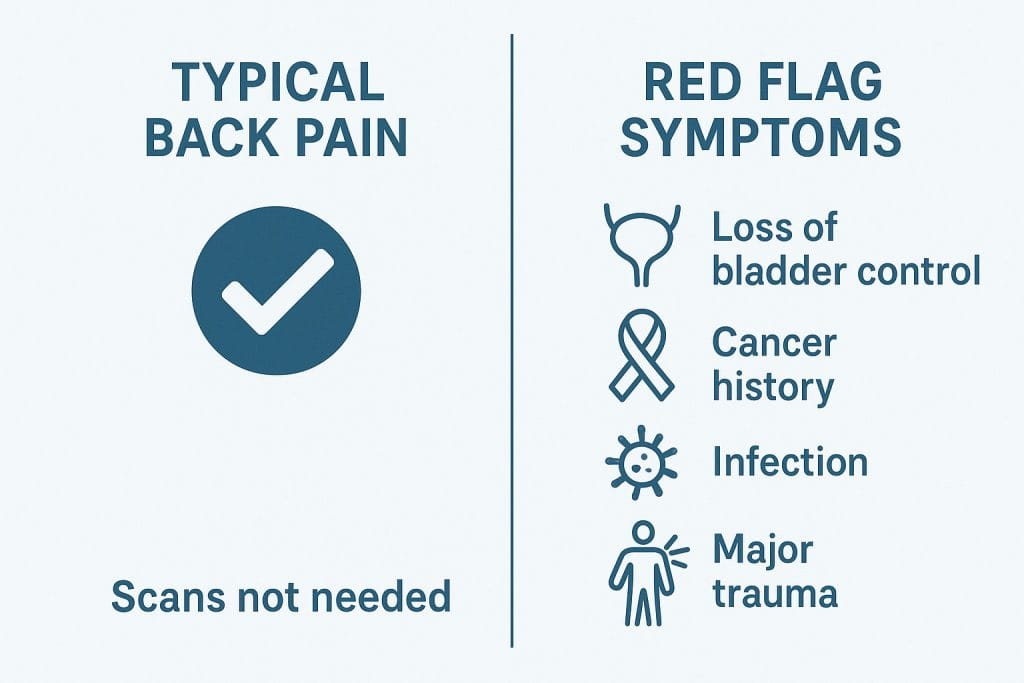
While routine scans aren’t usually necessary, they can be valuable in specific situations especially when there are warning signs of something more serious, such as:
- Loss of bladder or bowel control
- Significant weakness in the legs
- History of cancer
- Unexplained weight loss
- Fever or signs of infection
- Trauma (like a fall or accident)
In these cases, imaging can help rule out fractures, tumours, infections, or serious nerve damage. But for most people with typical lower back pain, scans add little value in diagnosis or treatment.
Understanding the path to recovery
If you’re dealing with back pain:
- Stay active: Gentle movement, walking, and stretching can help.
- Address stress: Mindfulness, breathing exercises, and relaxation techniques can reduce tension-related pain.
- Be patient: Most back pain improves with time and conservative care.
- Get support: A knowledgeable healthcare provider can help you understand your pain without over-relying on scans.
Final Thoughts
It’s frustrating to be in pain and not have a clear “cause” on a scan but it’s also a good sign. It means there’s no serious damage and that you have a good chance of recovery through active, non-invasive approaches. Understanding that back pain is often not visible on imaging can empower you to focus on what really helps: movement, mindset, and support.
Book an appointment with On Path Physio today, and let’s get you moving in the right direction without unnecessary setbacks.